Introduction
General chatbots are improving in their sophistication and are becoming increasingly capable of retaining context across multiple chat episodes with a user. This advancement is leading to an enhanced experience for users; however, simply storing information about prior searches and interactions is insufficient for the type of nuanced interaction required when working with those who struggle with mental health conditions. In the domain of mental health, memory must account for how a person changes—not just what they said. For an accurate portrayal of the user, this information must be derived from multiple inputs including clinical records (e.g., demographics; past medical/treatment history; provider notes; session transcripts; assessments) and frequent, often daily engagements that are indicators of behavior or symptoms (e.g., live texting/calling, journaling, sleep patterns, movement data). This depth and sensitivity exceed typical foundation‑model chat logs and requires representing emotional nuance, temporal layering, and interdependence with life circumstances (finances, health, employment, housing). Memory must track: shifts in affective valence and salience; the evolution of relationships; past vs. current states and recovery trajectories; recurrence patterns; and how coping capacity, detail density, time‑orientation (present vs. future‑focus), usage patterns, and cognitive distortion frequencies change. Simply “storing facts” or prompting queries with longer contexts fails to capture these mental health signals.
In this piece, we will explain how helping people with mental health needs must be handled differently.
Recent memory developments for consumer products
Most consumer products from frontier labs now contain persistent user memory with virtually unlimited context windows. For example, ChatGPT references prior chats, documents, and saved memories. Anthropic introduced Claude Memory with project‑scoped summaries and incognito mode, and Gemini added automatic personalization from past chats. In summary, these AI products save lots of facts and previous searches.
Other consumer products, like Character.AI and Janitor.AI, have leveraged clever UI to allow users to mark specific messages as pinned memories, enabling users to craft the assistant’s view of themselves on the platform.
There is wide evidence of people using genAI products for mental health support, and likely being a (if not the) leading usage of it, both for ChatGPT and for Claude. This begs the question: are current AI memory systems adequate for providing meaningful mental health support?
Why Mental Health Must Be Handled Differently
Current memory usage is largely about storing facts, but that is essential, and it is far from enough in a mental health context. Memory must track shifts in affective valence and salience, the evolution of relationships, past versus current states, recovery trajectories, and recurrence patterns. It must also be able to assess coping capacity, time orientation (present versus future focus), usage patterns, and cognitive distortion changes to adapt. Mere factual storage or context-heavy prompting fails to capture critical mental health signals such as emotional patterns, therapeutic readiness, and process-level changes. Below, we explore these challenges in depth.
Pacing is Hard
Therapeutic impact depends on timing. Even an effective technique can fail—or harm—if delivered when the patient isn’t receptive. For an LLM, choosing when to invoke a memory means:
- Avoiding overuse and intrusive recall
- Preventing harm to users from irrelevant or poorly used memories
- Guarding against outdated information that erodes trust
- Ensuring interventions reflect current reality, not resolved past issues
- Surfacing topics that are ready to discuss, while deferring those that aren’t
- Mimicking human “check‑ins” that build rapport without pressure
- Reaching the patient at moments of maximal availability and receptivity
This pacing must operate on two horizons: (a) macro readiness windows (e.g., a month of openness to practicing CBT), and (b) just‑in‑time micro‑windows that maximize response likelihood (e.g., brief periods when the patient is already on their phone). During the course of psychotherapy, macro windows can often be inferred through generalized and continuous interactions with the LLM, as well as specific patterns of engagement that indicate patient involvement with provided treatments. In contrast, just-in-time micro windows can be very nuanced and sensitive to patient context. For example, unpredictable events like relationship breakups or periods of high phone utilization for other purposes (e.g., social media) might be leveraged to optimize receptivity to treatment.
For a person struggling with a mental health condition, memories can either help or harm, depending on how often and when they are used during a macro or micro window. For example, outdated facts can undermine trust as users feel disconnected from what is happening in their lives. Alternatively, premature references to traumatic events might retraumatize a user before they’re ready to process a difficult episode. Additionally, retrieving memories with excessive frequency is likely to feel invasive and will result in a poor outcome.
Given these nuances, the timing of outreach and the application of appropriate memories is critical. Effective care requires (i) process‑aware memory (patterns of thought/affect/behavior) rather than mere content and (ii) pacing intelligence that detects month‑long “openness windows” (e.g., readiness for CBT practice) as well as just‑in‑time micro‑windows when the patient is most receptive (e.g., device‑use patterns). Our Chapter 3 methods describe how Jimini weights recency vs. reliability, models user readiness, and builds from factual recall to schema-level insights.
Process vs. content.
Good providers remember people and events, but real change comes from addressing process—the recurring patterns of thinking, feeling, and behaving that get triggered by life content. These patterns are often implicit and rooted in early adverse experiences that harden into maladaptive schemas. Example: a patient who shuts down whenever they feel threatened, echoing early caregiver dynamics.
Optimal memory use keeps awareness of content but prioritizes surfacing these patterns so they can be worked on directly. Changing a process typically requires two steps: (1) making it visible to the patient, and (2) targeted practice to install a healthier alternative.
The following examples will help to elucidate these principles:
Example 1 — Past heartbreak, new relationship.
Context: Last year, the user had a painful breakup with John; now she is struggling with a new relationship with Chris.
- Wrong (shaming, anticipatory): “Do a restructuring exercise before you talk to Chris, so you don’t repeat your past mistakes.”
- Why it's wrong: This weaponizes memory and implies the inevitability of repeated behavior.
- Right (reinforcement after success): After the patient uses a skill and has a good talk with Chris, reflect on growth: “You voiced your needs clearly—that’s real progress.”
- Why it’s right: It links content to process (assertive communication) and times recall to reward mastery, not to predict failure.
We build on this example in Figure 1.
Example 2 — Cancer worry and mis‑targeted support.
Context: The user has possible breast cancer with a follow‑up scan next week. She has a history of anxiety/panic.
- Wrong (logistics spam): Daily insurance reminders despite prior evidence of strong planning skills.
- Why it’s wrong: This increases the salience of fear and misses the emotional need.
- Right (emotion‑focused, invitational): “Hi Sarah, wondering how you’re feeling today. I’m here to listen if you’d like.”
- Why it’s right: Memory of her coping style drives emotion‑focused outreach with gentle optionality and appropriate cadence.
Example 3 — New schizophrenia diagnosis; grief curve.
Context: The user has auditory hallucinations and is depressed about their identity and future.
- Wrong (gratitude push): “Every day brings positivity!”
- Why it's wrong: This ignores the normative grief/adjustment curve; poor pacing.
- Right (coping‑oriented empathy): “Adjusting to your diagnosis is hard; I’m here. How are you coping today?”
- Why it's right: It acknowledges reality from memory and invites either pragmatic (symptom management) or emotional content, matching process and stage.
Example 4 — Agoraphobia, early success, low med adherence.
Context: A user is taking new medications and forgetting doses; one successful grocery trip last week.
- Wrong (reminder‑only): “Did you take meds today?”
- Why it’s wrong: If prior data show that reminders don’t change behavior, this is a low-yield approach and may be perceived as annoying.
- Right (motivational reinforcement + elicitation): “Great job last week leaving the house! What might help another success this week?”
- Why it’s right: Uses positive reinforcement to boost self‑efficacy; if the patient proposes reminders/meds, adherence improves via autonomy and fit.
Why are these examples complex for Frontier Labs’ LLMs?
Unlike other genAI chatbot companies, Jimini Health is built to serve mental health patients. We are positioned to help patients by leveraging various sources of valuable and unique data: frequent, often daily engagements (live texting/calling, journaling, reminders, clinical exercises, psychoeducation), as well as clinical records (demographics; past medical/treatment history; provider notes; session transcripts; assessments). This rich contextual information enables us to provide personalized care that adapts to each patient's evolving therapeutic journey.
Possessing rich data isn’t sufficient; clinical value depends on using it in context and time. As stated, the same intervention can help or harm depending on timing and the patient's current state. We recognize that patients evolve over time, requiring us to understand not just who they are today but their journey. We must accurately assess their current emotional state to determine appropriate support: Do they need compassion or motivation? Are they ready to confront difficult issues or need more preparation? These nuanced capabilities aren't necessary for general chatbots but are essential for effective mental health care.
To deliver therapeutic care, our assistant, Sage, relies on rich, evolving data sources and a sophisticated memory system, as detailed in the chapters below. Chapter 2 outlines the key data we capture across patient and provider touchpoints, while Chapter 3 introduces our three-layer memory model and shows how these inputs are transformed into an evolving, clinically usable understanding.
Figure 1
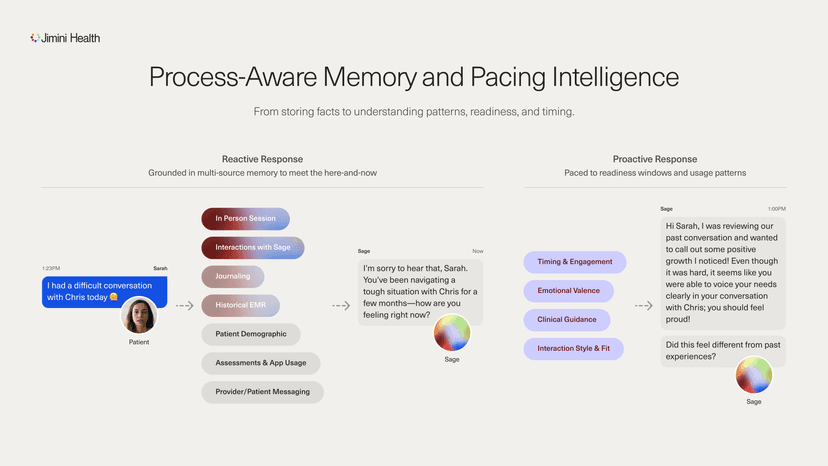
In the moment, Sage uses memory to help the patient feel understood without pushing a takeaway. Later in the week—timed for when the patient is typically open to engage (around 1 PM)—our assistant, Sage, follows up to highlight the growth (“you voiced your needs clearly”) and gently asks, “Did this feel different from past experiences?”
Data Relevant for Mental Health
Jimini's mental health system captures multidimensional patient data through complementary channels, creating a dynamic and evolving patient dataset that updates as circumstances change. Our system collects information from diverse sources, including:
- Provider Session Notes
- Conversations with Sage
- Conversations with Provider
- Patient Journal Entries
- Structured Clinical Exercises
- Therapeutic Goal Setting
- Integrated Medical Records
Beyond collecting data points, our system builds a nuanced understanding of the patient's social connections, emotional landscape, and life experiences. We track therapeutic progress alongside clinical treatment plans, revealing not just what treatments are applied but how they resonate with the patient over time. Our approach doesn't merely accumulate information—it builds understanding through varied perspectives on the patient's experience.
As shown in Figure 2, both provider interactions and patient engagements are enriched with comprehensive patient understanding. Information from these engagements is collected and fed back into each patient’s memory, creating a continuous therapeutic journey where each interaction builds upon previous context to form patient understanding.
For instance, when a patient expresses feeling overwhelmed, Sage can remind them of similar challenges they've overcome as well as surface specific coping techniques their providers previously recommended. Before the next session, Sage prepares a pre-session brief for the provider, maximizing session effectiveness.
This personalized support transforms moments of distress into opportunities for applying proven strategies, delivering confidence precisely when patients need it most. Simultaneously, the system works alongside providers without disrupting their workflow, but importantly, keeping providers fully informed of patient developments between sessions.
With the relevant data sources defined and organized, the next step is transformation. Chapter 3 presents our three-layer memory model and details how we structure, temporally order, and reconcile this information to produce clinically usable patient understanding.
Figure 2
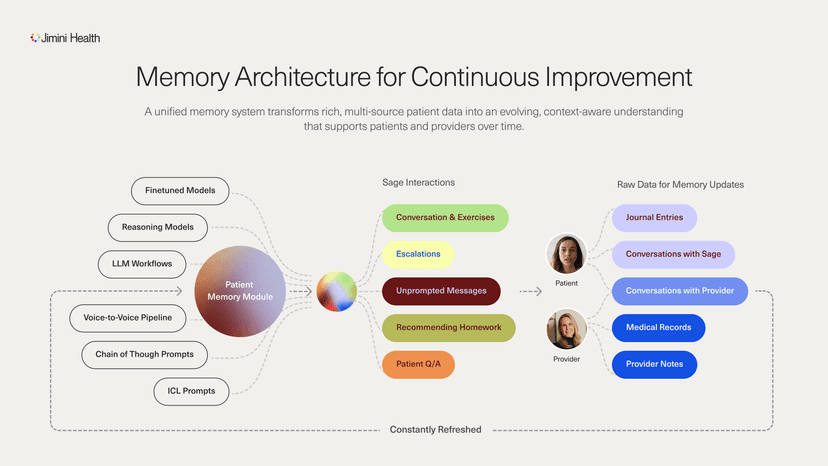
Jimini’s unified memory architecture connects multi-source patient data—journal entries, provider notes, provider and Sage conversations, and medical records—to a persistent patient understanding. This understanding supports both patients and providers, with each interaction enriching the memory for continuous improvement.
Memory Management Methods for Mental Health
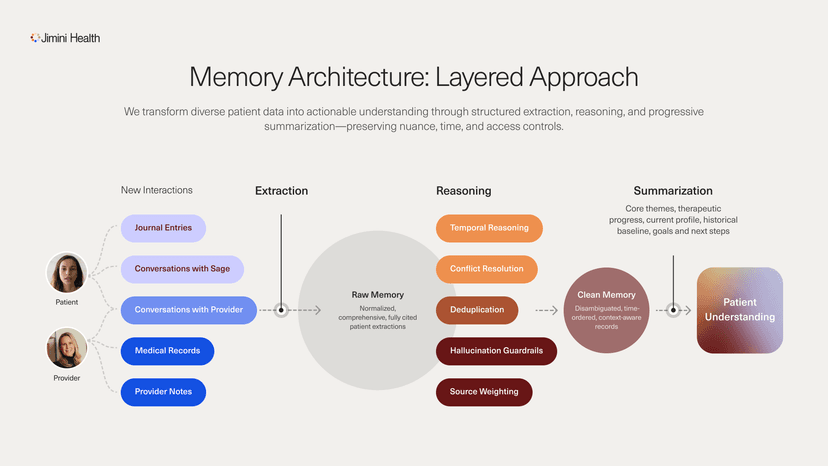
Building on the diverse data sources outlined in Chapter 2, our memory architecture transforms raw material into actionable intelligence. Figure 3 provides an overview of the layered pipeline that converts heterogeneous inputs into patient understanding.
Our process begins with a comprehensive extraction of clinical data from all patient interactions and documents on the platform. We transform unstructured information into structured data, creating a unified format that enhances reasoning. This foundational Raw Memory layer prioritizes completeness over selective relevance, capturing as much information as possible rather than prematurely filtering it. Each structured data point maintains citation links to its original sources, enabling complete traceability back to the raw data.
Structure is necessary but insufficient. Dumping structured facts into large context windows or leaning on similarity‑only retrieval misses the clinical nuance that mental health demands. Temporal order, in particular, reshapes meaning—whether “depressed” occurs before or after a noted improvement yields very different interpretations and next steps.
Content similarity alone is also insufficient. The same phrase—“I had a good day”—can carry radically different weight depending on who said it and when. For someone emerging from a depressive episode, it may mark a pivotal shift; for another, it’s baseline. Naïve similarity‑only retrieval, which ranks by lexical or embedding match without conditioning on patient context, time, or source authority will systematically miss that distinction.
We address these issues in two steps. First, we run a reasoning pass on newly collected Raw Memory to update the patient’s Clean Memory. As shown in Figure 3, this pass handles coreference resolution, deduplication, and temporal reasoning while balancing source authority with recency to resolve conflicts, remove clear hallucinations, and flag low‑confidence memories. It then prunes and distills older entries—merging them with newer records for journey context or condensing them when standalone. This progressive refinement preserves valuable history without becoming unwieldy, much like human memory favors essential meaning over verbatim detail.
Finally, we perform Summarization. This step assembles Clean Memory into concise, purpose‑built views—core themes, therapeutic progress, and current self. Together, these views form a rich patient understanding tapped to assist both patients and providers.
We also maintain explicit links between synthesized profiles and their source data. These links enable precise access controls—for example, ensuring our AI assistant, Sage, cannot surface treatment considerations from provider notes until the provider has discussed them with the patient. This aligns with the pacing principles from our earlier examples, preventing premature interventions that could cause harm.
Jimini’s memory system enables both providers and our AI systems to access a contextualized understanding of each patient that evolves alongside the patient’s journey—one that respects the temporal nature of human experience, the varying significance of different information sources, and the access patterns required by stakeholders in the patient’s care.
Figure 3
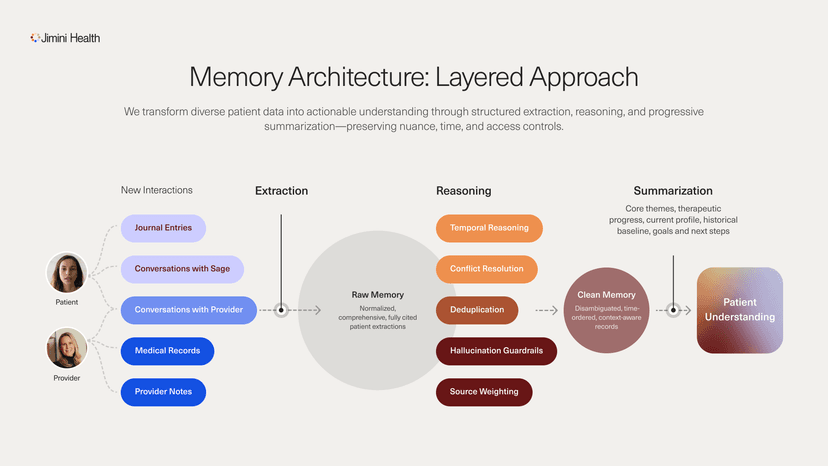
Memory Architecture: A layered pipeline from multi‑source data collection to Raw Memory (structured, cited facts), through a reasoning pass that disambiguates, orders in time, and reconciles sources into Clean Memory, followed by targeted summarization views—together producing an evolving, access‑controlled patient understanding.
* With contributions from: Tim Althoff, Johannes Eichstaedt, Bill Hudenko, Mark Jacobstein, Rahul Khanna, Ofri Raviv, Sahil Sud, Luis Voloch